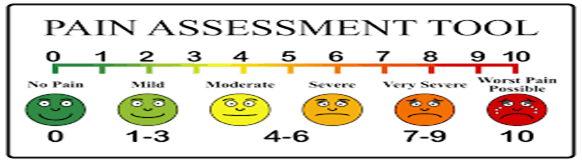
 Before being diagnosed with multiple autoimmune disorders and conditions, explaining my pain levels to a healthcare provider was easy. If I had a sprained wrist or a broken bone, they could see the injury. Using the 0 (no pain) to 10 ( the worst imagined) pain scale worked well most of the time.
Before being diagnosed with multiple autoimmune disorders and conditions, explaining my pain levels to a healthcare provider was easy. If I had a sprained wrist or a broken bone, they could see the injury. Using the 0 (no pain) to 10 ( the worst imagined) pain scale worked well most of the time.
All of that changed when living with daily pain became my new “normal”. Before I became chronically ill, I went weeks, days or years without physical pain. After I received a chronic illness diagnosis, good days would be when/if my pain level was 5 or less (mild to moderate pain levels). See: https://workerscompensationwatch.com/2018/01/08/im-a-10/
After life moved forward and my illness progressed with additional diseases and conditions, mild to moderate pain was never to be seen again. Daily pain levels became higher and my new normal changed along the way. Severe pain levels of 8 or more entered my life. Over the past thirty years, I have had to learn to live and function with pain levels that would have the average person bursting into tears.
This situation set off a whole new problem: most healthcare providers are taught to use standard pain assessment tools such as the Universal Pain Assessment Tool illustrated above. Many doubt and even dismiss my pain because “I don’t look like I should” as someone living with the reported high level of pain.
For example, I rarely cry when I experience the high pain levels; this can make explaining my pain levels difficult. Instead, I push through my pain and try to perform daily activities that would leave others immobile and non-functional. This causes others to doubt my pain experience.
I have often thought about how pain assessment tools could be adjusted to better meet the needs of those who live with chronic pain and illness. Could different pain tools be more useful for those living with persistent pain rather than the ones typically used for short-lived pain, such as that experienced after an operation or injury? I soon realized new tools are probably not the answer. The reason has to do with the differing experiences people have, even those “pain veterans” out there. Look, my pain score of 8 may be described by another as 5. Someone else reporting severe pain may be at a level considered mild for me. We know that as individuals, we process our pain differently; we can have the exact same diagnosis, but we each feel, cope, and manage our pain and symptoms differently.
Many people living with pain have had to learn to adapt to the pain, to work through the pain and still function. Just because we do not curl up in a sobbing mess when we are experiencing and reporting high pain levels does not mean we aren’t experiencing incredible amounts of pain. Honestly, many of us try to “master our pain” so we can at least appear to be “normal” like those who are blessed to live a relatively pain-free life.
Why? We had to learn how to protect ourselves and our emotions. We wish not to be ridiculed by family or friends for always being in pain or for cancelling plans once again because of the pain. Frankly, we work hard at hiding our pain around loved ones because we do not want them to worry about us. Plus, when we get upset or cry, our pain levels increase. Added stress can cause our symptoms to flare, and that causes our pain levels to rise too.
So here is my plea. The next time you hear a chronically ill person report they are experiencing level 8 pain on a daily basis, remember that not all of us show our pain in ways you might expect. Do not choose to dismiss us or refuse to believe us; instead, remember some of us have lived with pain for years and years and we struggled to learn to adapt.
How about considering asking some different questions, like:
- What is your daily pain level?
- Has it changed over time?
- Are you living with a higher vs. lower level of pain over recent ____(days, weeks, months, since your last visit)?
- Have you experienced stigma, being disbelieved, or criticized because of pain?
- What might I do to help you?
For those of you living with pain, caring and/or advocating for others with persistent pain: Please keep on fighting the good fight, all you brave and fabulous pain warriors! Try not to fear teaching others—your medical providers, family, and friends about your life with pain. You will make the difference for yourself and for others.
Further reading on TPC about pain assessment:

Great content! We should have the courage to face our problems and fight our pain.
Thanks!