Pain 101
“There is no one who loves pain itself, who seeks after it and wants to have it, simply because it is pain.”
 Fact or Fiction:
Fact or Fiction:
- Pain is just a symptom: False
- Pain is meant to “build character”: False
- Pain is complex and a subjective experience: True
- The experience of pain is unique to every individual: True
- Pain is common to most people: True
- Pain is a result of your past mistakes or a punishment for wrong doing: False
- Pain remains mysterious and requires more study: True
- Pain is the most frequent problem reported during hospital admissions: True
- There is a significant under-reporting and under-treatment of pain in minorities, women, children, and elderly: True
- Those diagnosed with terminal illness have reported that severe and unbearable pain is feared more than death: True
- Pain affects all aspects of a person’s life—including those around them: True; see chart
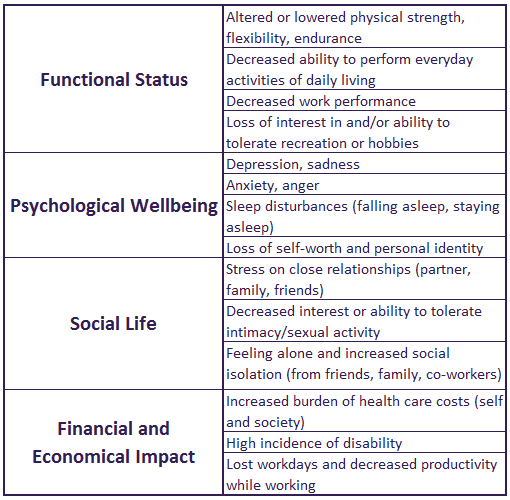
Source: modified from AGS Panel on Persistent Pain in Older Persons. J Am Geriatr Soc. 2002;50(6 Suppl):S205-S224.
Pain Definitions:
- Scientific Definition: An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage. [International Association for the Study of Pain (IASP); 1986]
- Clinical Definition: An uncomfortable sensation that bothers or upsets the person. “Pain is whatever the person says it is, occurring whenever the person says it hurts.” [Margo McCaffrey, RN, MS, FAAN; 1967]
Types of Pain:
Nature’s “red flag,” acute pain tells us that something is wrong from a disease or injury.
Cause: Generally known or quickly discovered. Common causes of acute pain: accidently injury or trauma, surgery, infection or inflammation.
Duration: Short-term, eases as healing takes place following correction of cause; usual course of pain is one to two weeks to less than three months.
Treatment: Focused on correcting the cause (example surgery or repair of injury); pain care should consist of variety of treatment options (medication and non-medication based) that are slowly reduced over time as pain lessens. More intense pain relief is often required for the first 48-72 hours depending on extent of injury or correction of disease.
Failure or Delayed Treatment: Uncontrolled acute pain can lead to the development of continued pain [chronic pain syndromes].
- When pain is uncontrolled, spontaneous impulses may arise from the nervous system, creating central sensitization;
- Hospitalized, seriously ill patients with high levels of pain are at risk for continuous pain for up to 6 months after discharge (St. Marie, ASPMN Core Curriculum, 2002)
Pain that occurs without apparent biological value that has persisted beyond the normal tissue healing time (IASP). It can be related to a previous injury or surgery, a medical condition or for no known reason.
Cause: Often unknown or can result from an acute injury where pain is not effectively treated or the nervous system does not normally adapt or respond (return to normalcy).
Duration: Continues after healing; fails to lessen over time; continues for three months or more
Treatment: Comprehensive, multi-disciplinary, multi-modality and integrative approaches to lessen pain, improve ability to function and minimize side effects are required; promoting change in lifestyle to include emphasis on wellness along with medication and non-medication based therapies may be most effective. TPC suggests that the pain care plan includes:
- Incorporating movement and exercise whenever possible
- Finding or re-discovering purpose and meaning to one’s life
- Establishing and maintaining social connection
- Improving diet towards healthy eating (colorful foods that have recently been living)
Adapted from David Rakel MD educational series.
Failure or Delayed Treatment: May contribute to more resistant pain conditions that fail to respond to treatment plans, undue and inhumane suffering, evolution of mental distress that could cause suicidal gestures, suicidal acts or other desperate behaviors, such a substance abuse as a means of self-medication.
Episodic pain that breaks through pain medications. Experts do not agree on whether this pain emerges with only one type of pain or one type of treatment plan. Breakthrough pain may occur when opioids are used (most common description), when other pain medication treatments are used (and opioids are not) or when multi-modality treatment plans are in use. Breakthrough pain was initially used to describe pain conditions that were caused by cancer—where most research and clinical applications for opioids have been used. BTP is reported in non-cancer related pain conditions too. Some state that BTP is different than “pain flares,” while others interchange the use of these terms.
Cause: Varies; breakthrough pain can be from an activity that causes pain or occur spontaneously with no known reason. Some health care providers state it can occur when the pain medication wears off before the next dose is due (end of dose failure).
Duration: Episodes can occur from 2-6 times per day; may peak within a minute and last from several minutes to an hour.
Treatment: Identify and address the cause; a health care provider may suggest you use a rescue medication. You and your health care provider should track when this occurs, how frequently, how rapidly it intensifies, what the sensation(s) feel like, how long the episodes last and what helps it resolve to achieve effective management.
Failure or Delayed Treatment: Can precipitate overall failure of the pain care plan as BTP can worsen over time which impedes function and initiates unnecessary suffering.
Episodes of pain that occur suddenly over a short period of time from hours, days or several weeks.
Cause: Varies; can be from weather changes, overuse or strenuous activities like starting a new exercise program, spring or holiday cleaning, traveling without rest breaks, increased stress, changes in hormone levels as with the menstrual cycle or menopause, lack of sleep, an injury or no apparent reason.
Duration: Episodes occur suddenly, last longer than BTP and usually are slow to resolve unless there is an adjustment in activity and additional comfort measures are used.
Treatment: Identify and address the cause; your health care provider may suggest a rescue medication. You and your health care provider should track when this occurs, how frequently, how rapidly it intensifies, what the sensation(s) feel like, how long the episodes last and what helps it resolve to achieve effective management.
Self-management tips to consider are:
- Find a place to rest. Observe the pain and its characteristics.
- Is this in a familiar location, does it feel typical to you yet more intense?
- Are you having any new sensations, like numbness or muscle weakness?
- Are new, unfamiliar symptoms occurring like fever, vomiting, shortness of breath, new pain sensations and pain in an unfamiliar location? If so, these should be reported.
- Have you experience this before? If so, what did you do to help ease the pain? Get out your comfort kit: use an ice pack, heating pad, warm shower or tub bath, massage the area, over the counter or prescription rescue medications as allowed, etc.
- Think about what might have caused this flare.
- What did you eat today?
- How well did you sleep?
- Did you just help your neighbor clean out their closet?
- Did you walk an extra mile today?
- Start a journal to document when pain flares occur so you can learn more about you–what causes you to have a flare, what works to relieve them and how you might avoid that experience again.
- Pace yourself. If your activity level has changed recently, return to a normal routine. Think about how to better balance your active life with rest throughout the day. When you decide to resume a more active schedule, do so gradually and work in frequent, short breaks.
- Immediately following a pain flare, consider reducing your activity by 25-50% for the first day or two before resuming your past routine. Add or increase stretching and walking.
- Develop more activities that help distract you from your pain, like watching funny movies or TV shows, listening to music that relaxes you or gives you joy, reading a good book or visiting with people who you enjoy.
- If you do not have a rescue comfort kit or medication plan for these events, discuss this with your health care provider at the next visit.
Failure or Delayed Treatment: Can precipitate overall failure of the pain care plan as pain flares can repeat and worsen over time, impeding function and causing unnecessary suffering.
